Since December 2019 a case of unidentified pneumonia was reported in Wuhan, Hubei Province, Peoples Republic of China, which resembles those of viral pneumonia. There are four types of Coronavirus: α-coronavirus (α-COV), β-coronavirus (β-COV), δ-coronavirus (δ-COV), ϒ-coronavirus (ϒ-COV). Previously six coronaviruses cause disease in human beings. After SARS-COV and MERS-COV, SARS-COV-2 is the seventh member of the coronavirus family.
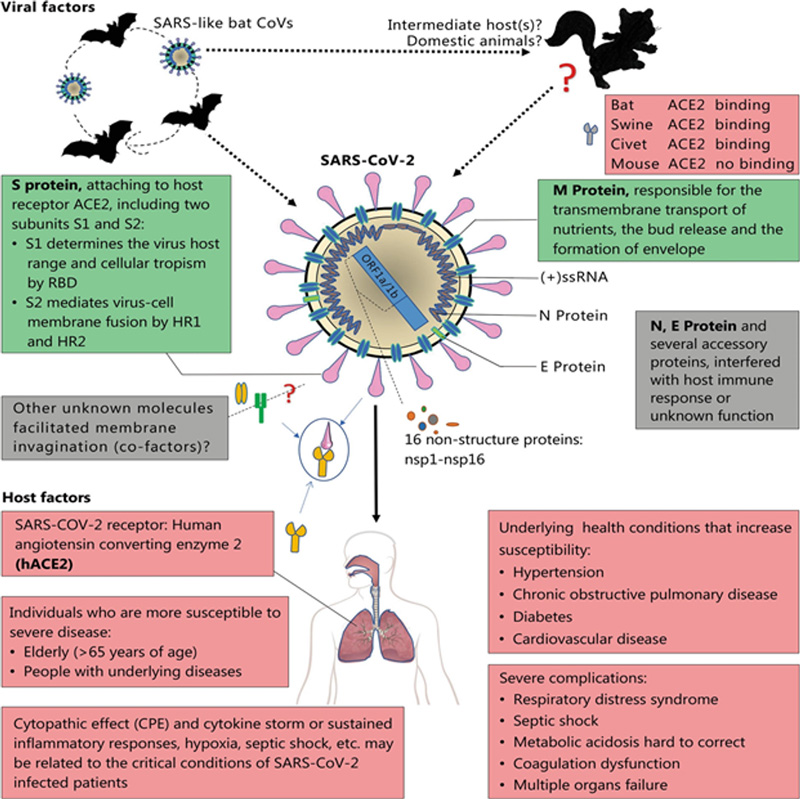
From five hospitalized patients, virus genome sequencing revealed the presence of a previously unknown β-COV strain in all of them. According to Li et al. (2020), β-CoV shows 88% similarity to the sequence of two bat-bat derived severe acute respiratory syndrome (SARS)-like coronaviruses, bat-SL-CoVZC45 and bat-SL-CoVZXC21, and about 50% identity to MERS-CoV. By the International Virus Classification Commission, β-CoV was named SARS-CoV-2.
The genome analysis of SARS-CoV-2 revealed that it contains 10 open reading frames (ORFs) — similar to that of typical CoVs. The first ORF is translated into two large poly-proteins and is about two-thirds of the viral RNA (21,290 bp).
Pathogenesis of SARS-CoV-2
S proteins of coronaviruses are a significant determinant of virus entry into the host cells. Membrane fusion and viral infectivity are mediated by proteolytic cleavage of SARS-CoV S protein at position (S2`). After entry into the host cell, the viral RNA genome is released into the cytoplasm and is translated into two polypeptides and structural proteins, after which the viral genome replication starts.
After insertion of newly formed envelope glycoproteins into the membrane of the endoplasmic reticulum or Golgi apparatus, the nucleocapsid is formed by the combination of genomic RNA and nucleocapsid proteins. The endoplasmic reticulum-Golgi intermediate compartment (ERGIC) is formed by viral particles. Then at last vesicles fuse with the membrane to release the viral particles.
Antigen presentation during infection
When the virus enters the cells, it would be presented to the central part of the body’s anti-viral immunity, antigen presentation cells (APCs). Mainly MHC-I molecule presents SARS-CoV antigen but the MHC-II molecule also contributes to its presentation. Previous research shows the susceptibility of SARS-CoV is correlated to numerous HLA polymorphisms, such as HLA-B*4601, HLA-B*0703, HLA-DRB1*1202, and HLA-Cw*0801. While some alleles are related to protecting against SARS-CoV infection, such as HLA-Cw 1502, HLA-A*0201, HLA-DR0301. Gene polymorphism of mannose-binding lectin (MBL), which is associated with antigen presentation, is related to the risk of SARS-CoV infection.
Studies revealed that there is a typical pattern of IgM and IgG production against SARS-CoV. IgG antibody lasts for a long time, while the IgM antibody disappears after 12 weeks which indicates that the IgG antibody plays a significant role. More researches have been done on cellular immunity in case of SARS-CoV infection than humoral response.
Main death cause of COVID-19 (SARS-CoV-2)
Immunopathological event of SARS-CoV-2, SARS, and MERS is ARDS (Acute respiratory distress syndrome), which is the main death cause among COVID-19 infected persons. Pro-inflammatory cytokines (IFN-α, IFN-ϒ, IL-1β, IL-6, IL-12, IL-18, TNF-α, etc.) and chemokines (CCL3, CCL5, CXCL8, CXCL9, CXCL10, etc.) are released in large amounts during the inflammatory response by immune effector cells in SARS-CoV infection.
A violent attack will be triggered by cytokine storm on the immune system causing multiple organ failure and ARDS and finally lead to death in severe cases of SARS-CoV-2 infection, according to previously published data.
How coronaviruses avoid immune responses?
Pattern recognition receptors (PRRs) recognize pathogen-associated molecular patterns (PAMPS), to detect dsRNA. SARS-CoV and MERS-CoV can avoid the detection of dsRNA by replicating in double-membrane vesicles. The antigen presentation can be affected by inhibition of the TFN-1 pathway. Besides accessory proteins, 4a of MERS-CoV block the induction of IFN.
Tests for the diagnosis of COVID-19 (SARS-CoV-2)
Signs and symptoms of SARS-CoV-2 are atypical such as cough, dyspnea, viral pneumonia, etc. Therefore, besides epidemiological history auxiliary examinations including nucleic acid detection, CT scan, immune response identification technology, and blood culture are important.
Conclusion
The causative agent of COVID-19 is highly infectious and can be transmitted through close contact and droplets. There is not any available treatment or vaccine. The need of the hour is to control the source of infection, cut off transmission routes. Whether an individual is infected with virus, re-infection, the severity of disease all depends upon viral factors (virus type, mutation, viral load, the viability of virus in vitro, etc.), human immune system factors (HLA genes), neuroendocrine-immune regulation, gender, age, and physical status.
Author: Sadaf, S. Bahauddin Zakariya University, Multan-Pakistan
Leave a Reply